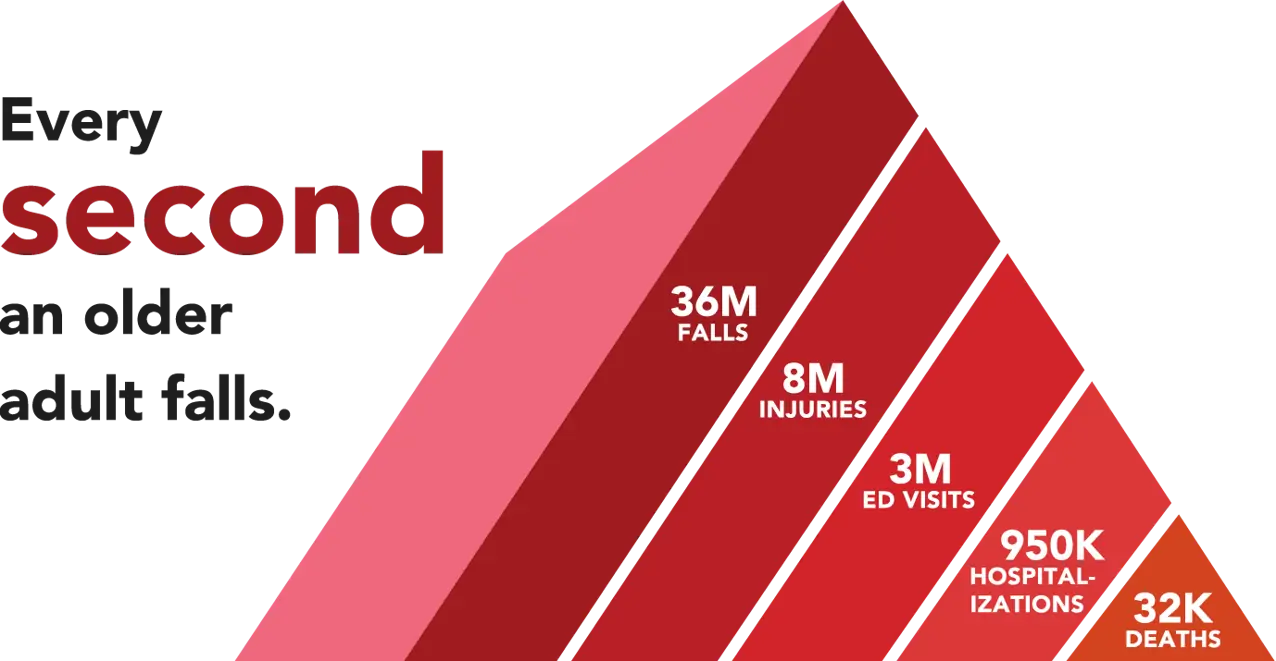
By the Numbers
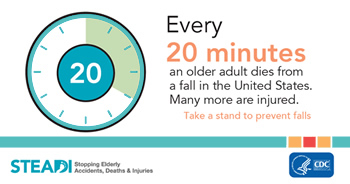
Falls are a major public health concern, particularly among older adults. According to the Centers for Disease Control and Prevention (CDC), more than one in four older people falls each year. Here are some facts about falls.
- 3 million older people are treated in the emergency department for fall injuries each year.
- More than 95% of hip fractures result from falls.
- In 2020, 29.1% of older adults in Minnesota (253,941) fell, resulting in 1230 deaths.
Have you sustained an injury from falling? Contact us today.
Fall Risks
Fall risks can be divided into several categories, including:
- Environmental factors: These include hazards in the physical environment that increase the risk of falls, such as poor lighting, uneven or slippery surfaces, cluttered spaces, and inadequate safety devices like handrails and grab bars.
- Health-related factors: Various medical conditions and medications can increase the risk of falls, including poor balance, muscle weakness, chronic pain, vision impairment, and cognitive impairment. Medications such as sedatives, tranquilizers, and some antidepressants can also increase the risk of falls.
- Behavioral factors: Lifestyle behaviors, such as physical inactivity, poor nutrition, alcohol consumption, and smoking, can increase the risk of falls.
- Psychosocial factors: These include factors related to mental health, such as depression, anxiety, and fear of falling. Psychosocial factors can lead to decreased mobility and physical activity, which can increase the risk of falls.
- Socioeconomic factors: Low income, limited access to healthcare, and social isolation can all contribute to an increased risk of falls among older adults.
By identifying and addressing the various categories of fall risks, healthcare providers and individuals can take proactive steps to reduce the risk of falls and prevent fall-related injuries.

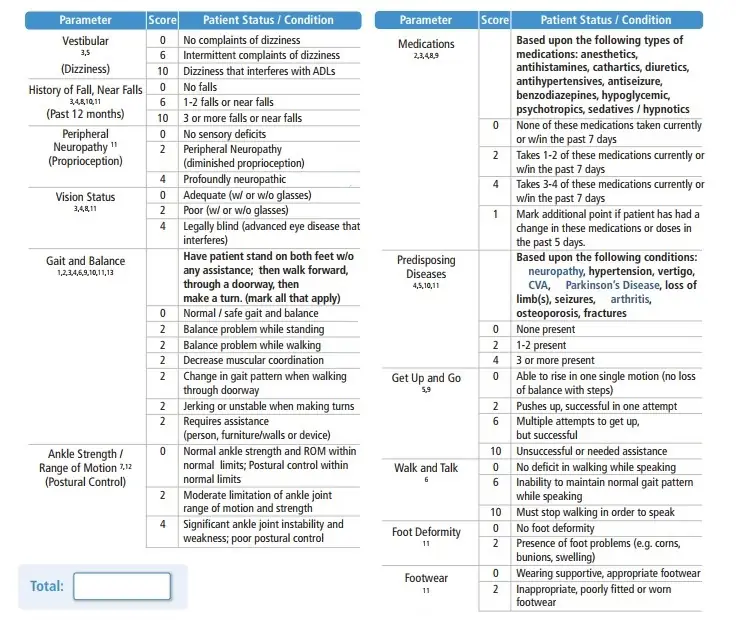
Fall Risk Assessment
Since fall is a complicated event, fall risk needs to be assessed with a multifactorial approach. There are many fall risk assessment tools. We adopt the Moore Balance Functional Fall Risk Assessment Tool for a whole person assessment with an emphasis on the lower extremity functions.
Lifestyle Medicine Approach to Fall Prevention
Fall prevention is an important aspect of maintaining good health and preventing injuries, especially among older adults. Lifestyle medicine can play a crucial role in fall prevention by focusing on lifestyle changes and interventions that reduce the risk of falls.
Here are some lifestyle medicine approaches that can help prevent falls:
Exercise: Regular physical activity can improve balance, strength, and flexibility, which are important factors in preventing falls. Strength training and balance exercises, such as yoga and Tai Chi, can be particularly effective in reducing fall risk.
Nutrition: A balanced diet that includes adequate amounts of calcium and vitamin D can help maintain strong bones and reduce the risk of fractures from falls. A plant-based diet can be an effective way to reduce fall risk in older adults.
Sleep hygiene: Adequate sleep is essential for maintaining physical and cognitive function, which are important in preventing falls. Lifestyle medicine practitioners can work with patients to address sleep problems and develop healthy sleep habits.
Passion, or having a strong sense of purpose and engagement in life, has been linked to a reduced risk of falls in older adults by improving physical activity, reducing stress, and improving self-efficacy.
Stress management: Chronic stress can increase the risk of falls by affecting balance and coordination. Lifestyle medicine approaches such as mindfulness meditation and relaxation techniques can help reduce stress and improve overall well-being.
Social connectedness: Social networks, or the relationships that individuals have with others in their community, can play an important role in reducing fall risk in older adults by increasing physical activity, improving mental health, and better access to resources.
Avoidance of harmful substances: Alcohol use can increase the risk of falls, especially in older adults. Alcohol affects balance, coordination, and reaction time, all of which are important for maintaining stability and preventing falls. In addition, alcohol can impair judgment and decision-making, leading to risky behaviors that increase the likelihood of falls.
Smoking can increase the risk of falls, especially in older adults. Smoking is a risk factor for a number of health problems, including lung disease, heart disease, and osteoporosis, all of which can increase the risk of falls. Smoking has also been shown to reduce bone mineral density, which can lead to fractures in case of a fall. In addition, smoking can cause peripheral neuropathy, which can impair balance and coordination and increase the risk of falls.
By taking a comprehensive approach to fall prevention that includes lifestyle medicine interventions, individuals can reduce their risk of falls and maintain their independence and quality of life.
Foot and Ankle in Fall Prevention
Foot pain can be a significant risk factor for falls, particularly in older adults. Foot pain can affect balance, gait, and overall mobility, increasing the risk of falls.
The ankle joint plays an essential role in maintaining balance during standing and walking. The ankle joint is responsible for providing stability, mobility, and proprioception to the lower limb. Proprioception is the body’s ability to sense its position and movements in space.
When the ankle joint is injured, such as in an ankle sprain or fracture, it can disrupt the normal functioning of the ankle joint, affecting balance and increasing the risk of falls. Ankle injuries can impair proprioception, leading to decreased balance control and increased postural sway.
Furthermore, ankle injuries can also cause muscle weakness, reduced ankle range of motion, and altered gait patterns, all of which can affect balance and increase fall risk. Proper rehabilitation and strengthening exercises are critical in restoring ankle function and reducing fall risk.
In older adults, ankle problems are a common cause of balance impairment, and regular physical activity that includes exercises that focus on improving ankle strength, balance, and mobility can help reduce the risk of falls and improve overall balance control.
Best Exercises to Reduce Fall Risks
There are several types of exercises that have been shown to be effective in reducing fall risk in older adults or individuals with certain medical conditions. Here are some examples:
Balance Exercises: These exercises can help improve balance and stability, which can reduce the risk of falling. Examples of balance exercises include standing on one leg, heel-to-toe walking, and standing on a foam pad with eyes closed.
Strength Training: Strengthening exercises can improve muscle strength and coordination, which can help reduce the risk of falls. Examples of strength training exercises include squats, lunges, and resistance band exercises.
Flexibility Exercises: Stretching and flexibility exercises can improve range of motion and flexibility, which can help reduce the risk of falls. Examples of flexibility exercises include calf stretches, hip stretches, and yoga.
Endurance Training: Endurance exercises can improve cardiovascular health and increase overall fitness, which can improve balance and reduce the risk of falls. Examples of endurance training exercises include brisk walking, cycling, and swimming.
It’s important to note that before starting any exercise program, it’s recommended to consult with a healthcare professional to determine the appropriate exercises and intensity for your specific needs and medical condition.
References:
1. Berg et al. Balance during standing, sitting to standing, one foot. Can.J.Pub.Health:83 (suppl.2):S7-11, 1992.
2. Boulgarides LK, McGinty SM, Willett JA, Barnes CW. Use of clinical and impairment-based tests to predict falls by community dwelling older adults. Phys Ther 2003; 83(4):328 – 39.
3. Brians LK, Alexander K, Grota P, Chen RWH, Dumas V. The Development of the RISK Tool for Fall Prevention. Rehabilitation Nursing, 16(2), 67- 69 (1991).
4. Freeman-Smith C, Bull K, Hough P, Greenwood K, Goldie P. Peninsula Health Falls prevention service; Rehabilitation, Aged and Palliative Care Services. The Peninsula Health Falls Prevention Service developed the Falls Risk Assessment Tool (FRAT) for a DHS funded project in 1999. A study evaluating the reliability and validity of the FRAT has been presented at a number of conferences, and is being prepared for publication. Meds, medical condition, history of falling, vision
5. Hendrich AL, Bender PS, Nyhuis A. Validation of the Hendrich II Fall Risk Model: A Large Concurrent CASE/Control Study of Hospitalized Patients. Applied Nursing Research, 16(1), 9-21 (2003).
6. Lundin-Olsson L, Nyberg L, Gustafson Y. “Stops walking when talking” as a predictor of falls in
elderly people. Lancet. 1997;349:617
7. Maki BE, Holliday PJ, Topper K. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol A Biol Sci Med Sci 1994;49: M72 – 84.
8. Morse JM, Morse RM, Tylko SJ. Development of a scale to identify the fall-prone patient. Canadian Journal on Aging, 1989 8,366-377.
9. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–8.
10. Poe SS, Cvach M, Dawson PB, Straus H, Hill EE. The Johns Hopkins Fall Risk Assessment Tool: postimplementation evaluation. J Nurs Care Qual. 2007 Oct-Dec;22(4):293-8.
11. Russell MA, Hill KD, Day, LM , Blackberry, I, et al. Development of the Falls Risk for Older People in the Community (FROPCom) screening tool Age Ageing (2009) 38(1): 40-46 doi:10.1093/ageing/afn196. This assessment tool was developed initially for use with hospitalized older people (the Falls Risk for Hospitalised Older People – the FRHOP). The FRHOP has been shown to have high retest and inter-rater reliability, and to have moderate ability to predict falls in older people in hospital (Australasian Journal of Podiatric Medicine, 2004: 99-108)
12. Sherrington C, Lord SR, Close JC, Barraclough E, Taylor M, O’Rourke S, et al. A simple tool predicted probability of falling after aged care inpatient rehabilitation. J Clin Epidemiol. 2011 Jul;64(7):779-86. Epub 2011 Jan 19.
13. Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 1994;331:821–7.
